Most recently updated July 7th, 2023
Estimated Reading Time: 18 minutes
If you live in the South, you know all about the annual yellow haze that hangs in the air and the yellow dust that covers every surface in the Spring.
This year we’ve had an especially prolonged pine pollen season. It started in February, and was still going strong in early April.
If you’re lucky, it’s just annoying.

Other people spend weeks this time every year wheezing and sneezing and taking LOTS of allergy meds.
Still another group of people (who never used to wheeze or sneeze in the Spring) find that they suddenly HAVE become allergic to the pervasive yellow dust….or something else, like, say bee stings.
How can that be? What happened?
The truth is that allergies and asthma, including what your triggers are, can change over time and strike without warning.
I experienced an unexpected new allergy earlier this year, with frightening and nearly deadly results!
Read on to learn more about my death-defying experience, plus how allergies change, and what you can do about it.
NOTE: I’m not a medical practitioner, and speak only from my own personal experience and what I’ve found in research. As always, consult your doctor before making substantial changes in your medications or habits.

The Asthma and Allergy Foundation of America (AAFA) calls allergies “among the country’s most common, but overlooked, diseases.”
WARNING: Before I get started, you should know this post is full of LOTS of sciencey stuff, which you may find useful but also boring. If you stick with me, though, you’ll also hear a tale of death-defying danger (and possible deadly stupidity) before we’re done.
How do You Get Allergies?
No one is born with allergies already in place.
Allergies happen when your body reacts to a harmless substance like pollen, animal dander, dust mites or specific foods.
Your body mistakes the allergen for a dangerous intruder and mounts a defense – a chemical called histamine – that causes symptoms of an allergic reaction.
But, according to Donna Sharpe, M.D., of Duke Otolaryngology in Durham, North Carolina, you can inherit atopy – the genetic tendency to develop allergies – from your parents.

-
-
- Even if your parents DON’T have any allergies, there’s still 15% chance that you’ll have them.
- If one parent is allergic there is a 20-40% chance of their children developing allergies.
- This increases to 60-80% if both parents are allergic.
-
And if you’ve inherited that trait, your allergies will become activated on your first encounter with pollen, animal dander, dust mites, or mold.
You probably won’t feel any symptoms the first time you run into those triggers, but that’s when your immune system starts making antibodies to fight them.

This is what’s known as immunological memory. Normally this is a helpful immune response which enables your body to respond quickly.
(This is also the immune function that is responsible for natural immunity to disease and allows traditional vaccines to work.)
In allergies, the immune response to a trigger is magnified, and causes your immune system to over-react.
So this is why you’ll have symptoms like wheezing, sneezing, and even more life-threatening reactions like severe asthma or anaphylaxis the next time you run into an allergen.

Allergies Through Your Lifetime
Allergies in Children
 Most people develop allergy symptoms between ages 2 and 18. Infants and toddlers usually start with skin-related symptoms like eczema.
Most people develop allergy symptoms between ages 2 and 18. Infants and toddlers usually start with skin-related symptoms like eczema.
About 60% of kids with eczema outgrow it, but they have a good chance of getting respiratory symptoms or asthma later on.
 In fact, according to a study in the Journal of Allergy and Clinical Immunology, about 20-30% of people with allergic asthma had eczema as a child.
In fact, according to a study in the Journal of Allergy and Clinical Immunology, about 20-30% of people with allergic asthma had eczema as a child.
Allergies as a Young Adult
 A lot of people seem to lose their allergies in their college years – but that may just be because they’ve moved away from what they’re allergic to!
A lot of people seem to lose their allergies in their college years – but that may just be because they’ve moved away from what they’re allergic to!
Of course, you could also move somewhere that makes you feel worse…
You won’t start feeling symptoms of new allergies until you’ve lived somewhere new for about a year.
Allergies as a Mature Adult
More life changes – in geography or living situations – happen throughout our adult years and can revive long-dormant allergies or create brand-new ones.
Your best bet is to see your doctor for any new allergy symptoms you can’t control with methods that worked for you in the past.
Allergy testing can help you identify exactly what’s triggering your latest symptoms so you can figure out how to avoid it.
Allergies As You Grow Older
 Your immune system produces less allergy antibodies as you get older, so you may have fewer symptoms.
Your immune system produces less allergy antibodies as you get older, so you may have fewer symptoms.
But you’re never too old to develop a new allergy; changes in location or living situation can still launch a new allergy or revive an old one.
Asthma and allergies are closely related, both in the triggers that cause them and in some of the responses of your immune system.

Asthma and Allergies
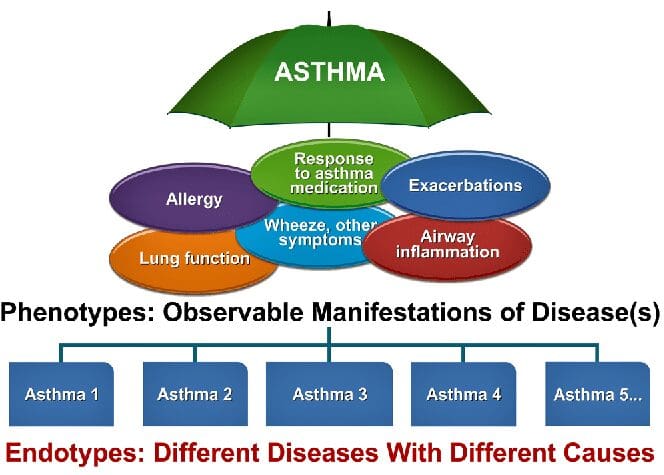
It used to be that “asthma” was just a big general bucket, but in the last couple of decades some basic types of asthma have been medically acknowledged.
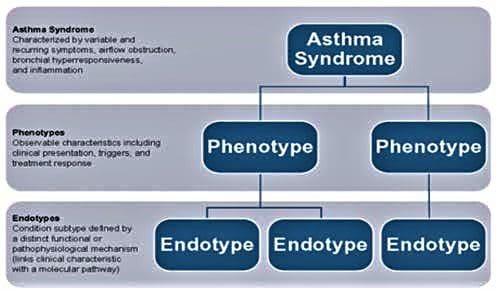
The two main accepted phenotypes (subgroups) of asthma used to be Allergic (Extrinsic) asthma and Non-Allergic (Intrinsic) asthma.
I say “used to be” , because now they just refer to these groups as Allergic asthma and Intrinsic asthma – which they have broken down into even smaller groups.
So now asthma is recognized as a spectrum of diseases caused by multiple environmental and genetic factors. Severe asthma is one form of the disease.
Mine is mixed, so I have severe asthma that is both Allergic and Non-Allergic. Yay 🙁

Intrinsic asthma is a lifelong condition that a person can control by using medication – but the risk will never really go away.
Allergic (extrinsic) asthma is a situational or seasonal response that disappears as soon as the trigger goes away.
Allergic asthma behaves very much like other allergies, except the allergic reaction includes classic asthma breathing problems that can be severe or life-threatening.

There’s no specific test that tells you what your subgroup (phenotype) is.
Subgroup diagnosis is usually left to your Doctor – hopefully based on discussion with you about your triggers and symptoms, and maybe some skin or blood tests.
A person’s subgroup (aka phenotype) may also change over time, which makes it even harder for doctors to understand and effectively treat your asthma.
It’s important to find a doctor who will listen to you and is up to date on the latest treatments!
I know this is tedious, but the more specific you can be about what is causing your asthma, the more effective your treatments can be. Okay, let’s keep going!

Drilling Down: What’s an Endotype?
So now we’ve got asthma subgroups (phenotypes), and breaking those subgroups down further we get to “endotypes”.
There can be several different endotypes included in the same subgroup.
Unlike subgroups, there ARE tests to find specific cells or molecules in your blood or spit that will define what your Endotype is.
Endotypes don’t change, because the types of cells, or inflammation present, won’t change – it’s actually part of your unique bodily makeup.
Here are two examples of endotypes in the TH2 (severe asthma) group:
Eosinophilic Asthma
Eosinophilscause airway inflammation. Their levels increase when you’re exposed to your asthma triggers, and then decrease. When they stay elevated between attacks they can cause severe asthma.
This type of asthma responds well to corticosteroids and other traditional asthma medicines.
Neutrophilic Asthma
Neutrophils also cause airway inflammation. This endotype isn’t understood very well yet.
It does NOT respond well to corticosteroids and other traditional asthma medicines, which can lead to severe asthma.
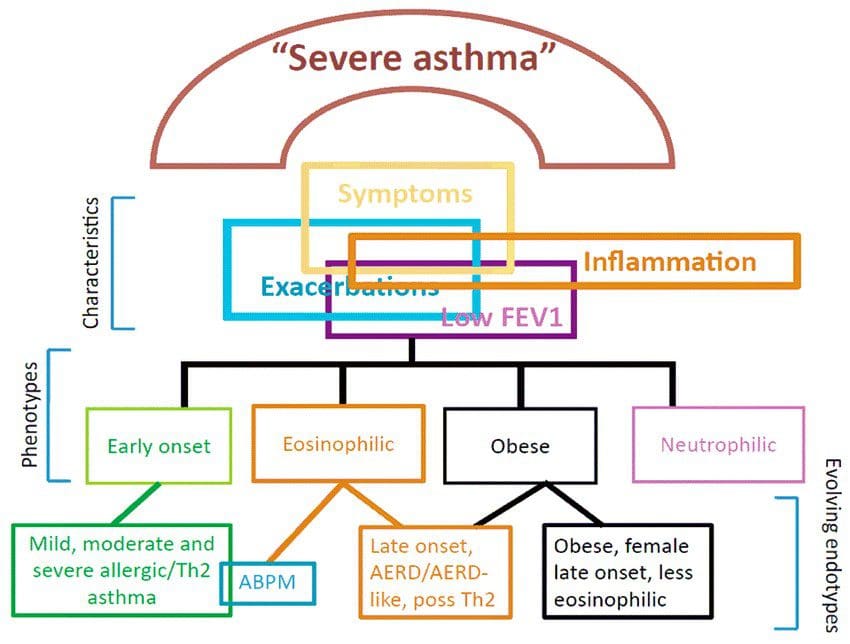
Phenotypes aren’t totally defined or understood at this point because they’re still learning about asthma genes and how they cause asthma.
Each person’s asthma is unique to them, which is why diagnoses and treatment needs the doctor and patient working together.

You Never Can Tell With Bees
Okay, now we’ve got a little bit of the sciencey background, I promised you a near-death allergic experience.
You’ve been very patient. Thank you 🙂
I labeled this section “You Never Can tell with Bees”, but in my head I think of it as “how a Jerk Wasp ruined 3 months of my life”.
Before I get started, I just want to say it took me FOREVER to write this post.
Not just because I wanted to be clear with all of the sciencey parts, but also because this was a frightening experience and could easily have gone VERY badly.
I don’t usually dwell on these kinds of things, I just absorb the hit and move on. But it’s a pretty good story. 🙂
What Had Happened Was….
So, it was a beautiful Monday afternoon in late September, and I was taking a moment away from my desk to enjoy the sunshine from my backyard deck.
Suddenly – WHAM!! Something bit me on the shoulder.
Out of the corner of my eye, I spied a wasp speeding away. Jerk wasp…
I didn’t think much of it, but returned to my desk. A minute later, the palms of my hands got very red and itchy.
Hmmmmm…. I took a hit on my inhaler, popped a Benadryl and kept working.
A couple of minutes later, my mouth was tingling. Uh-oh…..
I lifted my shirt in the mirror, and saw hives had erupted up and down my sides, and it was then I noticed hives all over my forearms, too.
My hands had swollen up like Mickey Mouse hands.
Now I started to get alarmed.
I had an Epi-pen for extreme asthma attacks, but my lungs were fine – it was just that my tongue was getting bigger and bigger – so I didn’t use it.
Instead, I got on the phone to my doctor’s office.
And went through a long automated answer tree….and waited on hold for what seemed like forever…..
When the doc finally got on the line, I found it hard to speak because my tongue had swollen so much.
Her advice: Call 911!
Having experienced the whole 911 thing before, I knew I didn’t have that kind of time.
I was within 3 miles of 2 different Emergency Rooms, so I got in my car and drove myself to one.
When I arrived at the hospital, there were no parking spots near the entrance, so I parked in the far lot and walk/jogged to the ER entrance.
By then, I couldn’t breathe, but the nurse at the desk wanted me to put on a mask and answer questions.
Fortunately, an ER doc had seen me come in, grabbed me, and took me to the back.
Two Epi-pen shots, oxygen, IV meds, 10 hours (and $5k) later, they let me go home.
The worst danger was over, and my lungs were never involved (weird, right?).
But I was what they call “twitchy” – that is very susceptible to more dangerous asthma attacks and anaphylactic relapse – for the next week.
I was forced to cancel outdoor performance plans (I sing at festivals) and stay in filtered air.
A couple of weeks later, I had another performance weekend at an outdoor event and thought I could do it.
As soon as we got there and I breathed the air, I knew it was a mistake.
I had a scary weekend, but made it through by using every trick at my disposal. The audience never knew 😉
A couple of weeks of terrible asthma passed.
Then, just as I was coming out of it, the asthma turned into a lung infection – which meant no singing (or hiking, either) for a good long time.
-
-
-
- The ordeal took me from the sting in late September until I could sing again by late November.
- In early December, I trained myself back up for a few weeks and was able to start leading hikes again in January (just in time for my annual “8 Weeks to Awesome” hike training!)
-
-
The whole experience was the opposite of fun, but I did learn some things.
And I admit I made a couple of nearly deadly mistakes:
-
-
-
- I didn’t use my Epi-pen at home.
- I didn’t call 911 or go to the ER immediately.
-
-
In my defense, I’d never had that kind of reaction to a sting before, and didn’t know I was deathly allergic to insect venom.
Now I know.
According to the American College of Allergy, Asthma & Immunology (ACAAI), the number of people who have allergies to insect stings is on the rise.
Apparently, now I’m one of them.
Thousands of people each year also need to seek medical help for severe reactions to flying insect stings. (This also includes me.)
Of those, the ACAAI says between 90-100 people each year die from insect sting anaphylaxis. (Thank goodness, NOT me!)

Allergies to Stings
The first time you’re stung – just like the first time you run into any other type of allergen – you probably won’t have much of a reaction.
But if you get stung again in the next few weeks, or you’re stung multiple times the next time, you’ll likely have an allergic reaction.
:max_bytes(150000):strip_icc():format(webp)/how-do-i-know-which-kind-of-insect-i-was-stung-by-82828-5c4e3f1cc9e77c0001d7bae4.png)
I’d only been stung once previously, about 15 years before my recent sting, but it was enough to give me a severe response.
So, what seems like a sudden allergy may have been there for years, waiting to respond to more exposure.
In fact, most fatalities due to bee stings occur in people who don’t even know they’re allergic.
Is It Anaphylaxis?
If you’re allergic to insect venom, anaphylaxis – a severe reaction – can develop within minutes to hours after you’re stung.
Around 5% of all people will have a severe allergic reaction to a sting – but how do you know if it’s anaphylaxis?
If you’re unsure, look for any or all of the following symptoms:
-
-
- Itching over the entire body
- Hives or swelling spreading from the site of the sting
- Flushing (reddening of the skin)
- A runny nose, sneezing, or postnasal drip (mucus in the throat)
- Itchy, watery eyes
- Swelling of the lips, tongue, and/or throat
- Shortness of breath, wheezing, and/or coughing
- Stomach cramping, nausea, vomiting, and/or diarrhea
- Lightheadedness, increase in heart rate, low blood pressure, or passing out
- A sense of panic or sense of impending doom
- A metallic taste in the mouth
-
I’ve highlighted in yellow the symptoms I had – and if I hadn’t sought help pretty quickly, I may have had more of them.
Though, TBH, these days an “impending sense of doom” could just be part of my world-view 😉

When to Seek Medical Attention
Don’t wait for symptoms to get worse – call 911 at the first sign of anaphylaxis. (I called my doctor’s emergency line first, and they told me the same thing,)
When it comes treating anaphylaxis in the moments after a sting, epinephrine is the treatment of choice.
Epinephrine is the drug form of the hormone adrenaline that your own body produces. It reverses the symptoms of anaphylaxis by increasing blood flow, opening your airways, and more.
If you have an EpiPen or AUVI-Q, inject it right away, then go to the hospital. (If you need a refresher, read How to Safely Use an EpiPen here. )
Anaphylaxis can return even after treatment, so they’ll probably want to monitor you at the hospital for a little while.

If you do have a bee encounter, your best defense is to cover your face and run!

Why, Jerk Wasp, Why???
You know I’m always asking “why” and trying to get more details about any of my adventures in asthma, and my encounter with the Jerk Wasp is no exception.
So, what did I learn from my experience with the Jerk Wasp and subsequent cascade of bad health consequences?
One of the more interesting parts of the Jerk Wasp adventure was that while I had an immediate and severe anaphylactic response to the sting, my lungs never reacted.
But, what does that mean? I’ve had anaphylactic asthma response before, but this was not that….
The video below explains the science behind extreme bee sting reactions. I like the video because it explains everything in an understandable way.
Plus, the professor is kind of funny 🙂
How to Manage Your Allergies
Allergies (and allergic asthma) can’t be cured, but they can be managed – even allergies to bee stings!
New allergies may take three to five years to develop, so if you haven’t had an allergy test recently, you may want to get one.
If you suspect you have any kind of allergy, talk with a healthcare provider before attempting to diagnose or treat yourself.
Common treatments for allergies include:
-
-
- Antihistamines.
- Allergy shots (immunotherapy) or drops.
- Avoidance of allergens or gradual sensitization to the allergen.
- Decongestants.
- Nasal sprays and nasal steroids.
-
Allergy shots and drops are the only current treatments that reduce sensitivity to an allergen itself, instead of just treating the symptoms.

The Most Common Allergies
Per the American College of Allergy, Asthma & Immunology, food allergies account for nearly 50% of the most frequent adult-onset allergies.
Peanuts, shellfish, and tree nuts triggered the most allergies.
The American Academy of Allergy, Asthma & Immunology or AAAAI found that younger children (aged 1-3 years old) were also getting more food allergies.
Why does this happen? The verdict is still out.
But I wonder if it has something to do with all of the additives and artificial modifications that are increasingly prevalent in the food supply….

Prevent Your Asthma & Allergies from Getting Worse
When it comes to controlling asthma and allergy symptoms, prevention can go a long way.
Keeping your home allergen free is one way to stay healthy.
Air Purifier Guide
If you want to be sure that your lungs and breathing are the best they can be inside your home, check out this helpful guide from ConsumersAdvocate.org on the air purifier industry.
More things you can do to help prevent asthma and allergy attacks:
-
- Take your asthma and allergy medications as prescribed.
- Cover your nose and mouth when spending time outside in allergy season
- Make sure you keep your indoor air free of allergens

I’ve included links to sources and references throughout this post, but here are few more if you want them!
Difference Between Extrinsic Asthma and Intrinsic Asthma

I hope this information about allergies and how they relate to asthma helps you in improving your breathing and your overall health!
If you’re battling asthma and allergies, you might be interested in these other posts:
Asthma’s Effects on Mental Health
What’s the Best Medicine for Your Asthma?
Asthma and COVID-19: Are You at Higher Risk?
Clean Your Indoor Air With Houseplants!
Fight Asthma with Vitamins and Supplements
Eat to Breathe Easier – the Best Food for Asthma
Hiking With Asthma! A 3-Step Plan for Success
If you have a question, drop me an email and I’ll reply as soon as I can. Thanks for stopping by – see you next time! LJ
To Get New Idratherwalk Posts
sent directly to your inbox (how convenient!) Click this Button
If you like this post, please share it!

LJ has spent much of her free time as a single Mom – and now as an empty-nester – hiking in the US and around the world. She shares lessons learned from adventures both local and in exotic locations, and tips on how to be active with asthma, plus travel, gear, and hike planning advice for parents hiking with kids and beginners of all ages. Read more on the About page.

