Most recently updated July 7th, 2023
Estimated Reading Time: 20 minutes
If you have asthma, like I do, you may be extra concerned about how COVID-19 could affect your health.
COVID-19, after all, is a respiratory disease and those of us with asthma have had bad experiences with those.
And by “concerned” I might also mean frightened, anxious, panicky… 😉
The COVID-19 virus is known to cause problems in the respiratory tract (nose, throat and lungs).

Because asthma is also a respiratory disease, it’s been assumed that people with asthma have a greater chance of catching the virus and getting very sick from it than other people.
It’s a reasonable assumption, and asthmatics have been classified as “high risk” since the beginning of the COVID-19 pandemic.
But I’m here to tell you, I’ve done the research, and at this point – maybe for the first time ever – asthmatics are just like everyone else 🙂
It’s important to know that currently there’s no evidence of increased COVID-19 infection rates in those with asthma.
And now, after months of studying this new disease, medical and infectious disease experts have been able to create a more exact picture of the risk to asthmatics.
Since the release of the vaccines, there have also been questions about the possible risk to people with allergic reactions. I’ll tell you what I found about the current CDC advice.
(I’ve included photos of my garden and places I’ve traveled, as a reminder both that while there is beauty to be found at home, the world is still full of amazing places waiting for us to find them!)
NOTE: I’m not a medical practitioner, and speak only from my own personal experience and what I’ve found in research. As always, consult your doctor before making substantial changes in your medications or habits.

COVID-19 and Asthma
Based on study findings published in The Journal of Allergy and Clinical Immunology, patients with asthma were found to be no more likely than those without asthma to be hospitalized for COVID-19.
Researchers noted that while this conclusion was unexpected, not all asthmatics are the same, so it may not apply to everyone with asthma.
In fact, in prior studies that analyzed patient risk by asthma subtype – allergic asthma vs. non-allergic asthma – those with non-allergic asthma were shown significantly more likely to have severe COVID-19.
This can be good news or not, depending on what type of asthma you have. Let’s take a quick review of what exactly asthma does to your body.

What Are the Symptoms of Asthma?
Asthma affects around 9.4% of children and 7.7% of adults in the United States. The symptoms range from fairly mild to life-threatening.
There is no cure, but some people do grow out of it, and medical drugs are available that treat the symptoms.
Many people with asthma do not feel sick, and can be very active until they run into something that triggers an asthmatic reaction.

WHAT ARE THE symptoms of asthma?
There are three main symptoms:
-
-
- Constriction of bronchial tubes (airways)
- Inflammation of lung tissue
- Thick mucus in the lungs
-
ASTHMA Treatment vs. ASTHMA Prevention
Asthma is a strange disease because many asthmatics feel fine most of the time – until you don’t, and then you need to act quickly!
But even when you do treat an attack successfully, lingering irritation can make your lungs more sensitive, and more likely to have another attack in the near future.

That’s where ongoing strategies for prevention – like maintenance medications, supplements, diet, and exercise come in.
It’s far better to prevent an asthma attack from ever happening, than to have to use emergency measures to treat a sudden attack.
What’s Your Asthma Type?
In many cases, asthma is a lifelong condition that a person can control by using a combination of medication and avoiding triggers – but the risk will never really go away.

In other cases, asthma is a situational or seasonal response that disappears as soon as the trigger goes away – and the good news is you can outgrow childhood asthma. 🙂
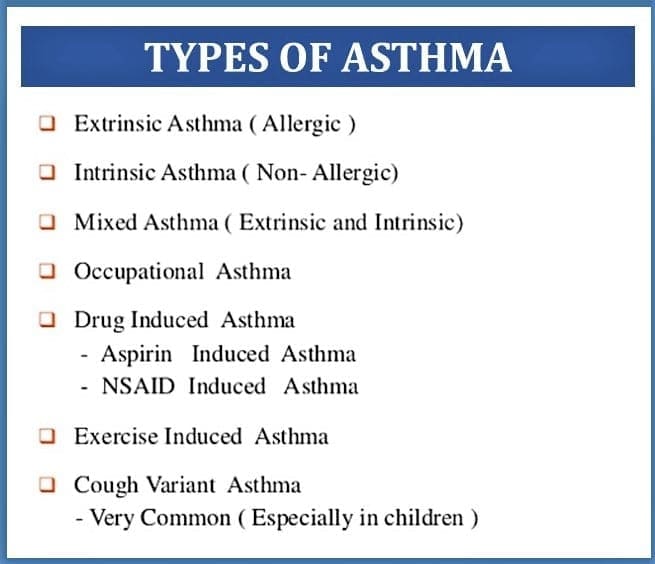
Types of Asthma
The two main types of asthma are Allergic (Extrinsic) asthma and Non-Allergic (Intrinsic) asthma.
Mine is mixed, so I have a combination of both Allergic and Non-Allergic. Yay 🙁
Allergic Asthma
Allergic (extrinsic) asthma is the most common type, affecting around 60% of people with asthma in the U.S.
Allergic asthma happens when the immune system overreacts to a harmless substance, such as plant pollens or house dust, by releasing an antibody called “IgE – immunoglobin E”.
The release of this antibody results in swelling (inflammation) and other asthma symptoms.
Around 8 in 10 people with allergic asthma will also have another allergic condition, such as eczema, allergic rhinitis, or a food allergy.
Nonallergic Asthma

Experts believe that nonallergic asthma develops due to genetic and environmental factors, so Nonallergic, or intrinsic, asthma doesn’t require an allergen to trigger an attack.
In fact, it can be hard to identify the potential trigger that results in intrinsic asthma .
Less common than allergic asthma, this type accounts for around 10–33% of all asthma cases. It’s more likely to appear in adulthood and affects more females than males.
Read more about these two types of asthma: Difference Between Extrinsic Asthma and Intrinsic Asthma

Risk of COVID-19 Infection in Asthmatics
Under normal circumstances, viral infections like COVID-19 are a big driver of flares in asthma patients.
But according to Linda Rogers, MD, of Icahn School of Medicine at Mount Sinai in New York City, research indicates asthma patients with COVID-19 don’t have any higher rate of hospitalization or mortality than other COVID-19 patients.
“As we look at data coming out of areas strongly affected by the pandemic, one very striking thing is the lack of high rates of patients with asthma having severe effects”, Rogers said.
As an example, she cited data from Wuhan, China, that shows asthma in < 1% of patients hospitalized for COVID-19, even though 5% of people in China have been diagnosed with asthma.
Rogers also cited mortality statistics from the New York State Department of Health, in which “asthma is not even in the top 10” comorbidities, even though 8%-10% of New York’s population has asthma.

But she cautioned that other factors could also explain these lower rates. For instance, patients with asthma may behave differently than patients with other chronic diseases, or it could be an artifact of how the data were collected.
Do additional conditions affect your risk of infection?
According to a team of Rutgers researchers, asthma does not appear to increase the risk for a person contracting COVID-19 or influence its severity.
In fact, asthma tends to be associated with far fewer other conditions than chronic obstructive pulmonary disease or cardiovascular disease.
“Older age and conditions such as heart disease, high blood pressure, chronic obstructive pulmonary disease, diabetes and obesity are reported risk factors for the development and progression of COVID-19,” said Reynold A. Panettieri Jr., a pulmonary critical care physician and director of the Rutgers Institute for Translational Medicine and Science and co-author of a paper published in the Journal of Allergy and Clinical Immunology.

“However, people with asthma — even those with diminished lung function who are being treated to manage asthmatic inflammation — seem to be no worse affected by SARS-CoV-2 than a non-asthmatic person. There is limited data as to why this is the case — if it is physiological or a result of the treatment to manage the inflammation.”
Does age play a role in how asthma patients react to the virus?

A person’s susceptibility to and severity of COVID-19 infection increases with age, whether or not they’re asthmatic.
COVID-19 causes dysfunction in the cells that line blood vessels throughout the body, so illnesses like diabetes, heart disease, obesity and other diseases associated with this condition may make people more susceptible to the virus than those who are just asthmatic.
That said, older people with asthma who also have high blood pressure, diabetes or heart disease may have similar instances of COVID-19 as non-asthmatics with those conditions.
Increased Risk of Complications?
Although the CDC states that patients with moderate-severe asthma could be at greater risk for more severe disease, there’s no published data at this point to support this determination.

“People with asthma are particularly vulnerable to viral respiratory tract infections because these infections can trigger an asthma attack, whether the infection is influenza, respiratory syncytial virus or coronavirus,” explains Christopher Hardy Fanta, MD, co-director of the Severe Asthma Program at Brigham and Women’s Hospital.

That said, in some people with moderate to severe asthma, COVID-19 may lead to pneumonia and respiratory disease – and viral pneumonia caused by COVID-19 may be difficult to manage in a person who has asthma.
“Remember: people with asthma get and survive the flu every year,” says Dr. Fanta.
“Even if you get COVID-19, you can get through a serious viral infection. The odds are very much in your favor.”
Non-allergic Asthma May Increase Risk
According to a new study led by researchers at Harvard T.H. Chan School of Public Health and Massachusetts General Hospital, adults with non-allergic asthma who became infected with COVID-19 were at higher risk of developing severe illness compared with adults who did not have asthma.
Allergy-induced asthma, according to the findings, did not significantly increase the risk of severe illness.
A pre-proof of the study was published online in The Journal of Allergy and Clinical Immunology on June 6, 2020.

“Despite reasonable speculation that asthma could be a risk factor for severe COVID-19, rigorous, population-based research is needed to know whether asthma and its major subtypes actually increase risk,” said Liming Liang, corresponding author of the study and associate professor of statistical genetics at Harvard Chan School.
“Based on these new findings, clinicians can improve risk-stratification and target COVID-19 prevention in patients with asthma, particularly those with non-allergic asthma.”
The Study
Since the start of the pandemic, clinicians have suspected that patients with asthma have increased susceptibility to COVID-19, but no longitudinal studies have analyzed the actual risk.
For the new study, the research team analyzed data from 492,768 participants in the UK Biobank, which stores biologic samples from participants and is linked to their medical records.
The researchers found 65,677 participants had asthma and 641 patients had severe COVID-19.
After adjusting for age, sex, body mass index, and other factors, the researchers found that having non-allergic asthma increased the risk of severe COVID-19 by as much as 48%.
They also found that the risk of severe COVID-19 increased by as much as 82% among people with asthma plus chronic obstructive pulmonary disease.
Importantly, however, the study showed that people with allergic asthma had no statistically significant association with severe COVID-19.
Zhaozhong Zhu, first author of the study and a research fellow at Harvard Chan School, noted that “the new findings are consistent with recent studies that have shown low levels of receptors for novel coronavirus (SARS-CoV-2) on the airway cells of individuals with allergic diseases and asthma.”
What this means is that people with allergies and allergic asthma may actually not possess the physical ability to get a severe COVID-19 illness.
The findings are especially important amidst allergy season, said study co-author Kohei Hasegawa, a physician at Massachusetts General Hospital’s Department of Emergency Medicine.
“This study should provide some reassurance during allergy season to the tens of millions of people with allergic asthma,” Hasegawa said.

How to Reduce Risk of Infection
According to Dr. Fanta, the best defense against serious illness is maintaining good asthma control.
This means people with asthma should keep taking all their daily asthma medications, including steroid inhalers.

Stopping a controller medication will put you at risk for developing a severe asthma attack.
What effect do inhaled steroids have on COVID-19?
Inhaled corticosteroids, which are commonly used to protect against asthma attacks, also may reduce the virus’s ability to establish an infection.
However, studies have shown that steroids may decrease the body’s immune response and worsen the inflammatory response.
Steroids also have been shown to delay the clearing of the SARS and MERS virus from the respiratory tract and so may also worsen COVID-19 outcomes.
Future studies should address whether inhaled steroids in patients with asthma or allergies increase or decrease the risks of infection, and whether these effects differ depending on the type of steroid used.

The bottom line for people with asthma during this pandemic is to keep doing what you’ve been doing all along—continue taking your controller medication and inform your healthcare provider of any symptoms that you may develop.
Should You Have the Vaccine?

Based on the available safety information today (June 2021), there are several valid criteria that may cause people to decide against or be advised against vaccination:
-
-
- A severe allergy or potential allergy to any of the ingredients
- Severe illness
- Pregnancy or breastfeeding, as data is lacking in these group
- An active COVID-19 infection or infection within the last 90 days
-
The CDC updated its guidance on December 30, 2020 with the chart below on how patients should be evaluated for eligibility to get the COVID-19 vaccination.
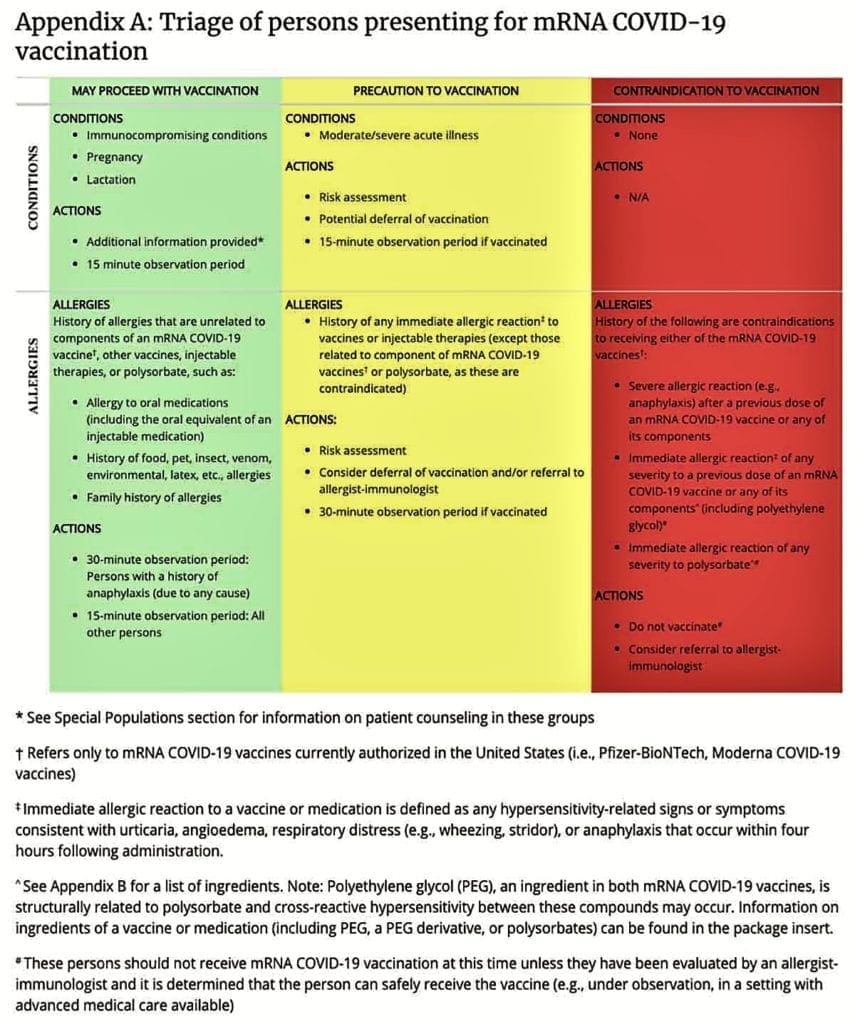
In summary, the CDC guidance says:
Who should receive the Pfizer/BioNTech or Moderna vaccine?
-
- Anyone with a history of food, insect venom, oral medications, environmental or latex allergies CAN get the vaccine
- Anyone with a family history of anaphylaxis not related to mRNA vaccines CAN get the vaccine
NOTE: You must undergo a 15-minute observation period (30 minutes if got a history of anaphylaxis) after receiving the vaccine to ensure there’s no allergic reaction.
Should you consult your doctor before getting the vaccine?
-
- If you have a history of anaphylaxis, or non-severe immediate allergic reactions to other vaccines, DO consult your doctor first.
NOTE: If you and your doctor decide you can receive the vaccine, you must undergo a 30-minute observation period after receiving it to ensure there’s no allergic reaction.
Who should NOT receive either of the vaccines?
-
- Anyone with a history of anaphylaxis to any component of the Pfizer/BioNTech or Moderna vaccines – basically anyone who has a reaction after the first dose of the vaccine – should NOT get the second dose.
- Anyone with a known history of non-severe immediate allergic reactions to any component of the vaccines should NOT get the vaccine.
- Anyone who is allergic to polyethylene glycol (PEG) or polysorbate should NOT get the vaccine. (PEG is a component in both vaccines; polysorbate is closely related to PEG.)
But what about the Covid-19 vaccine and asthma?
The current advice treats asthma just the same as any other kind of allergic reaction. They say:
-
- People with underlying medical conditions such as asthma can receive the COVID-19 vaccine as long as they have not had an immediate or severe allergic reaction to the vaccine or any of its ingredients.
I carry an Epi-pen and my anaphylactic response is severe enough to require intubation and placement on a ventilator.
I also don’t have any other co-morbidities, and I’m less than 60 years old. All that said, my doctor and I have decided that in my case it’s prudent to hold off on getting vaccinated for now.
Please consult with your doctor if you have questions about whether or not you should get the vaccine.

How to Manage COVID-19 with Asthma
You can manage a mild case of COVID-19 infection at home. It’s important to also self-quarantine to avoid spreading the infection to others.
“If you have COVID-19 infection, it’s best to use your inhaler to administer your asthma medication rather than your nebulizer,” advises Dr. Fanta. “Using a nebulizer would aerosolize the germ and spread it widely, like a whole series of uncovered coughs and sneezes.”
If you have COVID-19 symptoms or symptoms of another viral infection, your asthma isn’t under control and you find yourself short of breath following light exertion, it’s time to seek emergency medical attention.
“We do not know of any long-term harmful lung injury from COVID-19 infection,” says Dr. Fanta. “The assumption is that with recovery comes restoration of health, as is the case after the flu.”

How does the COVID-19 Virus Spread?
COVID-19 is a respiratory virus that is spread by droplets from coughs and sneezes and from touching infected surfaces.
As of posting date, we know that at least 80% of all people infected with COVID-19 will have only mild to moderate flu-like symptoms, including a fever and cough.
The remaining 20% may develop more severe cases of COVID-19, or may develop pneumonia or severe acute respiratory syndrome.
Generally, when a person contracts a respiratory virus, the infection sets the body’s immune response in motion.

In people with chronic asthma, this can lead to an overproduction of substances that only worsen inflammation.
COVID-19 is slightly different than other respiratory viruses in that it causes inflammation inside lung tissue, rather than the usual bronchial inflammation that occurs in asthma.
At present, there’s no evidence suggesting that people with asthma are any more likely to contract COVID-19 than anyone else.

How Does COVID-19 Affect the Lungs?
Coronavirus can affect the upper respiratory system (nose, sinuses and throat) with flu-like symptoms, the lower respiratory system (airways and lungs) by causing cough with or without mucous and difficulty breathing.
When COVID-19 is severe it can bring on pneumonia or acute respiratory distress syndrome (ARDS).
Upper Respiratory Infection
Common symptoms of respiratory infections in the nose, sinuses and throat include nasal congestion, runny nose, sore throat, sneezing, achy muscles and headache. Coronavirus upper respiratory infection symptoms also may include cough, diarrhea, fever, shortness of breath and tiredness.
Lower Respiratory Infection
Common symptoms of COVID-19 respiratory infections in the airways and lungs may include severe cough that produces mucous, shortness of breath, chest tightness and wheezing when you exhale.

When COVID-19 is Severe
When COVID-19 goes deep into the lungs, like other infections, it can cause pneumonia.
Pneumonia is a concern for older people because they have reduced lung capacity, require longer recovery time and have age-weakened immune systems.
Pneumonia that is caused by COVID-19 may be more severe, affect many parts of the lungs, and cause shock, organ damage, abnormal blood clotting, acute respiratory distress syndrome and deteriorating health.
How Pneumonia Affects the Lungs
When healthy lungs inhale, the lungs and their 480 million tiny air sacs (alveoli) fill with oxygen. These little air sacs allow you to get rid of carbon dioxide when you exhale, and pass oxygen into the blood vessels.

Pneumonia causes the air sacs to become infected and inflamed. This causes fluid and inflammatory cells to build up in the lungs and prevents oxygen from getting through, causing severe breathing difficulties and lack of oxygen in the blood.
Severe cases of COVID-19-related pneumonia are treated in the hospital.
Symptoms of Pneumonia Due to COVID-19
-
-
- Fever
- Fatigue
- Cough (with and without mucous)
- Loss of appetite
- Muscle aches
- Significant shortness of breath
- Chest pain (especially under the breastbone)
- Rapid breathing
- Sweats
- Headache
- Weakness
-

Acute Respiratory Distress Syndrome (ARDS)
Acute respiratory distress syndrome (ARDS) is a life-threatening injury to the lungs caused by infection or trauma.
ARDS causes fluid to leak into the lungs, making it extremely difficult to breathe.
It also causes a significant lack of oxygen in the bloodstream, which harms the brain, organs and body tissues.

Most people who develop ARDS are already patients in the hospital. Treatment includes:
-
-
- Oxygen therapy to ensure the blood and body have enough oxygen to function properly.
- Sedation to prevent agitation and shortness of breath.
- Fluids are managed to prevent build up in the lungs.
- If necessary, an extracorporeal membrane oxygenation (ECMO) machine may be used to oxygenate the blood outside the body while the body fights the infection and repairs itself.
- Pulmonary rehabilitation to help ARDS patients recover strength.
-

Asthma and Long COVID
COVID-19 has seen many respiratory specialists working together to tackle the immediate crisis, through waves of the initial outbreak and including the effort to understand the emerging syndrome of Long COVID.
Long COVID
Long COVID describes the effects of Covid-19 that continue for weeks or months beyond the initial illness.
The National Institute for Health and Care Excellence (NICE) defines Long COVID as lasting for more than 12 weeks, although some people consider symptoms that last more than eight weeks to be Long COVID.
What Are the Symptoms?
Researchers analyzed symptom data reported on the COVID Symptom Study app and identified two main groups of symptoms:
-
- One is mainly respiratory, such as a cough and breathlessness, and also includes fatigue and headaches.
- The second group of symptoms affects other parts of the body, including the heart, brain and the gut.
In the study of 4,182 people, heart symptoms such as palpitations or increased heartbeat were common, along with pins and needles, numbness and ‘brain fog’.

What’s the Recovery Time?
The study above, led by Leicester researchers, suggests that for those who were hospitalized for the initial illness, it’s common for Long COVID to last five months or more.
There are other, separate reports of it lasting 12 months or more. This includes both people who needed hospitalization initially and those who didn’t.
It’s important to note that this lingering effect isn’t unique to COVID-19 – other viral illnesses symptoms can also stick around for quite a while.
Who Is At Risk?
Long COVID affects around 10% of 18-49 year olds who get COVID-19, increasing to 22% of people over 70 years old.
Researchers found that older people, women, and those who had five or more symptoms in the first week of becoming ill with COVID-19 were more likely to develop Long COVID.
The researchers also found people with asthma were more likely to develop Long COVID.
(This was the only clear link they found to existing health conditions in people who developed Long COVID.)
REFERENCE: Long Covid

Asthma and Face Masks
As we all return to work, school and public places, face coverings and masks have become recommended (or government mandated) daily accessories.
I hesitate to say anything about this at all, because the question of wearing masks has become at least as political as it is health-related.
While none of us wants to spread or catch COVID-19, wearing a face covering raises many questions for people with asthma.
Should Asthmatics Wear Masks?

Little is definitively known about how effective the use of masks is in controlling the spread of COVID-19 because no studies have yet been carried out specifically connecting this virus to mask use.
The current advice given on the WHO’s website is still not to use masks unless you have the virus and are at risk of infecting others, or looking after those who may be infected with COVID-19.
The CDC and the World Health Organization (WHO) both recommend that everyone wear masks or face coverings in public where you can’t “social distance”.
And, in quite a few States in the USA, citizens are required to wear face masks in public or face hefty fines.
The WHO also recommends wearing a fabric mask that allows you to breathe while talking and walking quickly.
The theory is that people who become infected can unknowingly spread the COVID-19 virus because they have few or no symptoms.
So wearing a mask can help prevent the spread of the disease.
“For people with very mild asthma or well-controlled asthma, it’s probably not going to be an issue,” said Dr. David Stukus, member of the Medical Scientific Council for the Asthma and Allergy Foundation of America (AAFA).

“For people who have very severe disease and have frequent exacerbations, ER visits, hospitalizations, require lots of medications and frequent symptoms, it might cause more issues for those folks.”
If you’re having trouble wearing a mask, but they’re required for your work or by government mandate in public where you live, try a different fabric or fit.
Wearing some kind of breathable face covering is better than nothing, and will meet requirements to allow you to work or shop for food.
Some mask-related triggers to watch for:
-
- Hot, humid weather and pollen can be asthma triggers. If you have asthma, you may need to be cautious while wearing face coverings during hot weather or when the pollen is high.
- Exercise is important for people with asthma. But wearing a mask while exercising vigorously may make it harder to breathe. Continue to stay active, but avoid crowded situations where you would need a mask.
Exercising outdoors in the sunshine is best 🙂

What If My Job Requires a Face Mask?
As you return to work, you may be required to wear a mask or face covering as part of your job. But if you have trouble breathing while wearing a face covering, what are your options?
The first step is to work with your employer. Talk about ways you can work without a mask while still helping prevent the spread of COVID-19.
People with asthma are covered under the Americans with Disabilities Act (ADA).
Under this act, people with disabilities can ask for reasonable accommodations so they can work. If your work requests won’t create a hardship for your employer, you can ask for accommodations.
But the ADA also says if an accommodation could cause harm to other people, then a business does not need to provide the accommodation.

So, if a person with asthma is coughing and not wearing a mask, an employer could require the person with asthma to stay home or wear a face mask/covering.
If your company requires a face mask or covering, try to find one that meets the requirements, but also allows you to breathe.
Thin fabric or a paper mask might work, or one that hangs like a veil (allowing more air flow).
Don’t be afraid to talk to your supervisor or human resources representative. They may also have some creative ideas to help you do your job while managing your asthma.

Summary
I’ve included a lot of information in this article about COVID-19 and how it can affect asthmatics. Here’s a quick summary of all we’ve covered:
-
- There’s no evidence that asthmatics are more likely to catch COVID-19 than non-asthmatics
- Allergy-induced asthma, according to findings, did not significantly increase the risk of severe COVID-19 related illness.
- Infected adults with non-allergic asthma had higher risk of developing severe illness than COVID-19 infected adults who did not have asthma.
- Asthma patients with COVID-19 don’t have any higher rate of hospitalization or mortality than other COVID-19 patients.
- A person’s susceptibility to and severity of COVID-19 infection increases with age, whether or not they’re asthmatic.
- People with asthma should keep taking all their daily asthma medications, including steroid inhalers.
- Do practice social distancing, wash your hands, get good outdoor exercise and eat a healthy diet.
- If you carry an Epi-pen for severe allergic reactions or are allergic to any component of the COVID vaccines, consult with your doctor before getting the shots.
- You can manage a mild COVID-19 infection at home, but know when to call your doctor.
- Severe cases of COVID-19-related pneumonia and ARDS must be treated in the hospital.
- Face masks may cause distress for some asthmatics, so wear a thin mask that allows air flow in situations where it is mandated or you can’t social distance.
I’ve included links to sources and references throughout this post, but here are few more if you want them!

REFERENCES:
“Association of asthma and its genetic predisposition with the risk of severe COVID-19,” Zhaozhong Zhu, Kohei Hasegawa, Baoshan Ma, Michimasa Fujiogi, Carlos A. Camargo,and Liming Liang, The Journal of Allergy and Clinical Immunology, June 6, 2020, doi: https://doi.org/10.1016/j.jaci.2020.06.001
Garg S, Kim L, Whitaker M, et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–464. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e3
https://www.nytimes.com/2020/04/16/health/coronavirus-asthma-risk.html
Air Purifier Guide
If you want to be sure that your lungs and breathing are the best they can be inside your home, check out this helpful guide from ConsumersAdvocate.org on the air purifier industry.

I hope this information about COVID-19 and how it relates to asthma helps you in improving your breathing and your overall health!
If you’re looking for ways to asthma-proof the air inside your home, read about Tips to Control Indoor Allergens and how you can Clean Your Indoor Air with Houseplants.
To learn about how what you eat (or don’t) can also improve your asthma, read about my Anti-Inflammatory Asthma Diet.
To read more articles about how to live better and be more active with asthma and allergies, check out How Asthma and Allergies Change Over Time and the Fitness and Wellness page.
If you have a question, drop me an email and I’ll reply as soon as I can. Thanks for stopping by – see you next time! LJ
To Get New Idratherwalk Posts
sent directly to your inbox (how convenient!) Click this Button
If you like this post, please share it!

LJ has spent much of her free time as a single Mom – and now as an empty-nester – hiking in the US and around the world. She shares lessons learned from adventures both local and in exotic locations, and tips on how to be active with asthma, plus travel, gear, and hike planning advice for parents hiking with kids and beginners of all ages. Read more on the About page.

