Most recently updated July 7th, 2023
Estimated Reading Time: 17 minutes
If you or your children are asthmatic, you’ve probably spent a lot of time looking for the best medicine for your asthma.
Or maybe looking for better asthma treatments, if you’ve already been prescribed something.

If you’ve read some of my other posts, you know that I’ve had asthma and have been fighting it my whole life, with both medical and non-medical tools.
In the U.S., asthma affects more than 25 million people.
There is no cure, but some people do “grow out” of it (meaning you don’t have obvious symptoms), and medical drugs are available that treat the symptoms for those that have them.
I didn’t grow out of it, and from childhood through young adulthood, my parents tried all available medical options to make my illness better.
But in spite of allergy shots and prescribed inhalers and pills, my asthma got worse every year.

Finally, as a young adult, I had an epic attack that led to complete respiratory failure and several days unconscious on a ventilator.
When I woke up, the doctors just told me to take more medicine and stay in a controlled environment.
That’s when I became very pro-active in my search for better treatments and lifestyle choices to reduce my asthma symptoms and prevent future severe attacks.

I’ve had some success 🙂
In this post I tell you about the prescribed medical options available now, and the ones I’ve used – and mostly still use – that appear to help my chronic asthma.
For inspiration I’m also sharing photos of beautiful places I’ve been able to hike, without any trouble breathing!
Some of my posts contain affiliate links. If you make a purchase through an affiliate link, I will receive a small payment at no additional cost to you. As an Amazon Associate, and other marketing affiliations, I earn from qualifying purchases. See full Disclosure page here.
The first step to getting some relief is figuring out what kind of asthma you or your kids have.
Asthma can affect the breathing of children or adults, and symptoms range from fairly mild to life-threatening.
NOTE: I am not a medical practitioner, and speak only from my own personal experience and what I’ve found in research. As always, consult your doctor before making substantial changes in your medications, exercise, or eating habits.

What Kind of Asthma Do You Have?
The easiest way to classify your asthma is to identify the things that cause an attack – i.e. your triggers.
Some Common Asthma Triggers:
-
-
- Smoke – cigarette and fire smoke
- Air Pollution – smog, car exhaust, other air pollution
- Chemicals in food
- Pet dander
- Pollen, Mold and Dust
- Food allergies
- Insect bites and stings
-
Prior to the 1900’s, it was generally agreed that asthma was caused by either an allergy or a mental disturbance of some kind.
Then in 1916 Francis Rackemann found that not all non-psychosomatic asthma was as a result of allergies.
(The psychosomatic theory has been largely discounted, but sadly, is seeing some resurgence. But that’s a story for another time….)

Allergic or Non-Allergic
He designated the two main categories of asthma as “intrinsic” (non-allergic) and “extrinsic” (allergic).
-
-
- Extrinsic asthma is your body’s reaction to an air-borne or ingested allergen.
- Intrinsic asthma is a reaction that does not include an external allergen.
-
You can have either kinds of asthma or both. I’m lucky enough to have both kinds 🙂
If you have allergies, your immune system produces antibodies to attack substances that generally cause no harm, such as pollen, dust mites and pet dander.
For asthmatics, our allergic immune response includes tightening and inflammation of airways, plus secretion of thick mucous in the lungs – making it very hard to breathe.
It wasn’t until 1921 that doctors also realized that most asthmatics have allergic reactions to both indoor AND outdoor irritants.
The asthmatic over-achieving immune system responds to other non-allergic (intrinsic) events in the same way.

World Asthma Day
World Asthma Day is held each May by the Global Initiative for Asthma, (GINA) (www.ginasthma.org), a World Health Organization (WHO) collaborative organization founded in 1993.
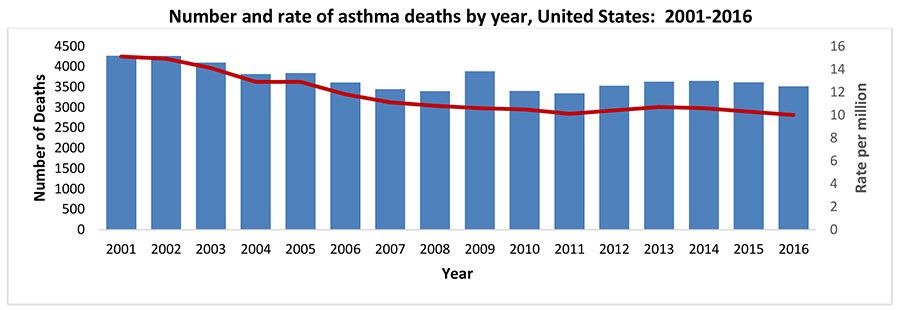
According to WHO, or is that whom? :-), it’s estimated that in 2016 alone more than 339 million people had asthma worldwide and there were 417,918 deaths due to asthma across the globe.
This year’s World Asthma Day theme was “Uncovering Asthma Misconceptions”. Learn more about World Asthma Day here.
There are many dangerous misconceptions about asthma, including that people “grow out” of their asthma.
People simply stop having asthma symptoms, they don’t grow out of it. But asthma symptoms can, and frequently do, return later in life.
-
-
-
- In women, birth control pills and hormonal changes during pregnancy or menopause can trigger a sudden return of asthma symptoms.
- Lifestyle changes, such as moving to a more polluted area, can also make asthma flare up again.
- Other breathing issues, such as COPD or emphysema, can be made worse by underlying asthma.
-
-
In the UK, 3 people die every day from asthma attacks. Many of these deaths could be prevented with proper use of treatments.
That said, there is a large group of people who still have bad symptoms, even if they take their medicine as prescribed.
This is because there are a few types of asthma that just don’t respond very well to current treatments.
In general, Intrinsic (non-allergic) asthma will require long-term control medicine of some kind and mild to moderate Extrinsic (allergic) asthma could be treated with only a rescue inhaler.
No matter what, asthmatics should try to avoid their known triggers whenever they can.

Asthma Medication Options
Long-term control treatments help you to avoid an asthma flare up. They should be taken even when you don’t have asthma symptoms.
Quick-relief medications are only for when you need them.
They’re called rescue inhalers because they act quickly to stop an attack that’s already happening.
Biologics are newer, injectable treatments you can use if other asthma treatments aren’t enough for you.
The types and doses of asthma medications you need depend on your symptoms, the severity of your asthma, and known medication side effects.
Asthma can change over time, so you should work closely with your doctor to track your symptoms and adjust your asthma medications, if needed.

NOTE: This section is long, and packed full of information that (of necessity) requires lots of potentially tiresome reading. I’ve tried to make it interesting with comments about my own experiences with each type of drug. 🙂
Long-term Control Medications
There are several types of long-term asthma control medications, including the following.
Inhaled corticosteroids
These anti-inflammatory drugs are the most effective and commonly used long-term control medications for asthma.
They reduce swelling and tightening in your airways. You may need to use these medications for several months before you get their maximum benefit.
Inhaled corticosteroids include:
-
-
-
- Fluticasone (Flovent HFA)
- Budesonide (Pulmicort Flexhaler)
- Mometasone (Asmanex Twisthaler)
- Beclomethasone (Qvar RediHaler)
- Ciclesonide (Alvesco)
-
-
Regular use of inhaled corticosteroids helps keep asthma attacks and other problems linked to poorly controlled asthma in check.
Leukotriene Modifiers
These medications block the effects of leukotrienes, immune system chemicals that cause asthma symptoms.
Leukotriene modifiers can help prevent asthma symptoms for up to 24 hours.
Leukotrine Modifiers include:
-
-
-
- Montelukast (Singulair)
- Zafirlukast (Accolate)
- Zileuton (Zyflo)
-
-
In rare cases, montelukast can be linked to psychological reactions, such as agitation, aggression, hallucinations, depression and suicidal thoughts.
Long-acting beta agonists (LABAs)
These bronchodilator medications open airways and reduce swelling for at least 12 hours.
LABAs are used on a regular schedule to control moderate to severe asthma and to prevent nighttime symptoms.
Though effective, they’ve also been linked to severe asthma attacks. To combat this, LABAs are taken only in combination with an inhaled corticosteroid.
The most commonly used LABA for asthma is salmeterol (Serevent).
I have been using Serevent for years with success, both in diskus and inhaler form.
Theophylline
You take this bronchodilator daily in pill form to treat mild asthma. The active ingredient is derived from a compound found in coffee.
I was prescribed Theophylline pills as a child through young adulthood, but usually didn’t take them until I needed them, and when I did they made me jittery.
Then, when I was in my 20’s and having an especially bad season, I started taking more of these pills and had to get frequent refills.
When the Pharmacist accused me of selling them (?!) I decided to:
-
-
- Get a new pharmacy and
- Investigate other treatment options.
-
It never occurred to me that anyone would take this stuff for fun. I hated taking so many pills…
That said, Theophylline relaxes the airways, decreases the lungs’ response to irritants and can be helpful for nighttime asthma symptoms.
If you need a quick home treatment for mild wheezing, try drinking some hot coffee – it will help ease your breathing 🙂
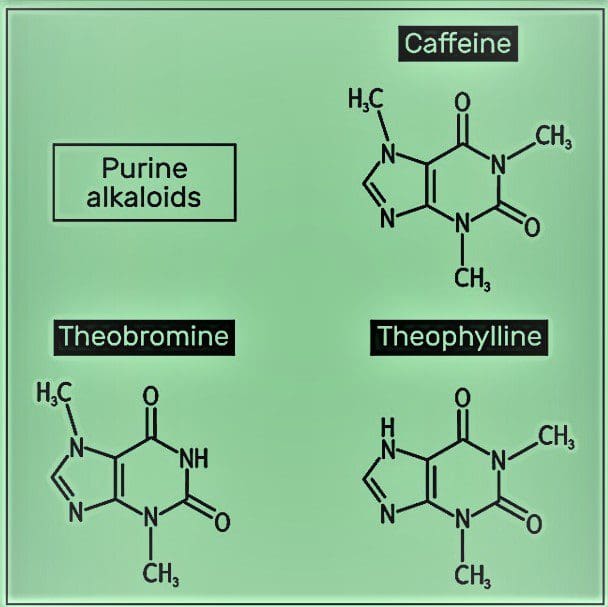
Theobromine
I recently found myself looking for a new bronchodilator medicine when I couldn’t get my regular prescription inhalers due to supply chain issues.
I found Theobromine, a mild bronchodilator related to Theophylline, sold as an over-the-counter supplement in capsule form.
Theobromine is milder than Theophylline and is often found as one of the ingredients in so-called “fat burning” diet supplements. But it’s also sold in capsules on it’s own as a dietary supplement.
Theobromine, related to both caffeine and theophylline, is a natural stimulant found in some foods, such as cocoa and chocolate (made with cocoa).
So, what does it do?
Theobromine Benefits
Theobromine, like caffeine and theophylline, acts as a stimulant to give energy. It also helps to alleviate sleepiness, and increases concentration and focus.
Those are nice benefits, but for my purpose in fighting asthma symptoms, I’m more interested in it’s abilities as a vasodilator (widens the blood vessels) and bronchodilator (increases lung function).
This stimulant can also benefit heart health and can have a positive effect on mental health by promoting a feeling of calm.
Chocolate is good for your teeth, and so is Theobromine! It helps harden tooth enamel to reduce the appearance of stains on our teeth.

Okay, so sparkly white teeth aren’t required for good lung function, but I’ll take it as a bonus 🙂
There are also many theobromine benefits you can get without taking pills – just eat the healthiest kind of chocolate.
Corticosteroids and LABA Combos
Some inhaled asthma medications are a combination of both a corticosteroid and a bronchodilator:
-
-
- Fluticasone and salmeterol (Advair Diskus)
- Budesonide and formoterol (Symbicort)
- Mometasone and formoterol (Dulera)
- Fluticasone and vilanterol (Breo)
-

Quick-relief Medications
Often called rescue medications, they can ease worsening symptoms or stop an asthma attack in progress by relaxing airway muscles.
They begin working within minutes and are effective for four to six hours.
Though not intended for daily use, some people use a quick-relief inhaler before exercise to help prevent asthma symptoms.
Quick-relief medications include:
-
-
- Albuterol (ProAir HFA, Ventolin HFA, others)
- Levalbuterol (Xopenex HFA)
-
If your symptoms are infrequent or you only have exercise-induced asthma, you might manage just using a rescue inhaler.
I have used both ProAir and Ventolin and found them equally effective, so to me that’s a choice to make based on cost.
Most people with persistent asthma also need an inhaled corticosteroid or other long-term control medication to go along with the rescue inhaler.
Ipratropium
Ipratropium (Atrovent HFA) is a short-acting bronchodilator usually prescribed for emphysema or chronic bronchitis, but sometimes used to treat asthma attacks, too. It may be used either with or instead of short-acting beta agonists.

Oral Corticosteroids (Pills)
These medications may be taken, usually in pill form, to treat severe asthma attacks.
Though inhaled steroids have few side-effects, these pills are a stronger dose and can cause annoying short-term side effects, and more-serious side effects if they’re taken for a long period.
Examples of these medicines include:
-
-
-
- Prednisone
- Methylprednisolone
-
-
Whether inhaled or taken in pill form, cortico-steroids are prescribed specifically to treat inflammation in the lungs.
I’ve only ever taken Prednisone following a hospitalization, and I hated them. Apparently my body did, too, because I would start throwing them up within 3 days of being discharged.
That said, sometimes you have to take strong medicine until you can breathe real-world air again. 😉
Steroid Side Effects
Because inhaled corticosteroids are used over the long term, side effects can be a concern.
Possible side effects include:
-
-
- Fungal infections,
- Hoarseness,
- Bruising, and
- Weight gain.
-
Long-term use of steroid asthma treatments in pill form can cause more serious side effects, including cataracts, thinning bones (osteoporosis), muscle weakness, decreased resistance to infection, high blood pressure, mood swings, and reduced growth in children.
In my case, I’m more sensitive than usual to even the relatively small doses of steroids in inhalers, so I opted not to take them as a preventive medicine.
When I was young, there were no other medical options for long-term treatment of asthmatic inflammation, but today we have more choices 🙂

Medication for Allergic Asthma
For most people, allergies are annoying and inconvenient, but for asthmatics an uncontrolled allergy can put us in the hospital.
Allergy Shots
Allergy shots (immunotherapy) may be an option if you have allergic asthma that can’t be controlled by avoiding triggers.
You’ll begin with skin tests to see which allergens trigger your asthma symptoms, then get a series of injections containing small doses of those allergens to create an immunity to it.
When I had these tests done, they drew a grid on my back, and then pricked the skin inside each box with a different type of allergen.
They measured the skin reaction of each applied allergen to see which things caused me the most trouble.
There were several clear winners, including grain dust, mold and pet dander.
I took allergy shots for several years, but I’m not sure they did any good.
But I’m not sure they didn’t either 😉
At the very least, the tests identified my triggers so I could take steps to avoid them.
Allergy Medications
Another thing you can do is take regular OTC allergy medications to help relieve your asthma.
These kinds of meds include oral and nasal spray antihistamines and decongestants, as well as corticosteroid and cromolyn nasal sprays.
Allergy medications are available over-the-counter and in prescription form.
I regularly take Benadryl pills in addition to my asthma meds to keep my lungs clear during allergy season.
Epinephrine Auto-Injectors
Also known by the trademark name “Epi-Pen”, these are syringes full of epinephrine (adrenaline) which is a powerful fast-acting bronchodilator.
You need a prescription to get one of these. They can be quite pricey, and expire within a year, so only get one if you really think you might need it.
This kind of treatment is recommended for people who have previously experienced and survived acute asthma attacks or non-asthmatic allergic anaphylaxis.
To use the syringe, you inject yourself in the thigh, and the correct dosage is administered automatically. I have one, and always carry it in my purse.
NOTE: You would only use this treatment if you have a known serious reaction. For wheezing alone, you would use your fast-acting inhaler. Talk to your Doc about whether or not you need one.
Be sure to hang on to the empty syringe and give it to the doctors at the hospital so they know how much medication you’ve taken.

Breathing Bad Air

One of the irritants that can trigger an attack is any kind of air pollution.
It could be pollen or dust, smog from cars or factories, fire or cigarette smoke, or even “bad ozone” trapped near the ground due to bad weather conditions.
More than half of people with asthma say that air pollution makes their symptoms worse, with potentially life-threatening consequences.
There’s also an established link between high pollution days and respiratory-related hospital admissions.
Growing evidence also suggests that air pollution can cause new incidences of asthma, and the levels of air pollution all over the world have been increasing every year.

Weather-Related Breathing Risks
We’ve talked about the yearly Pollening in the South, and the havoc it wreaks on people with allergies and asthma each Spring.
And where I live in North Carolina, you can pretty much count on several days to several weeks each summer of extreme heat and humidity, too.
Along with that sticky weather, comes a dangerous amount of “bad ozone” trapped close to the ground.
What is Bad Ozone?
The stratosphere (or ozone layer) extends upward from about 6-30 miles and protects life on Earth from the sun’s harmful ultraviolet (UV) rays. So that’s good.
But ozone on the Earth’s surface is a very poisonous gas. And that is bad.
Ground level ozone is harmful to breathe and damages crops, trees and other vegetation.
Near ground level, ozone is formed when pollutants emitted by cars, power plants, chemical plants, and other sources react in the presence of sunlight.
What Does Bad Ozone Do?
Ozone is a powerful oxidant that can irritate the airways, especially on hot sunny days when ozone can reach unhealthy levels.
Relatively low levels of ozone are enough to cause health effects – even if you don’t have asthma or other breathing problems.
People exposed to elevated levels of ozone may have irritated eyes, nose and throat.
They may also have respiratory or heart symptoms such as shortness of breath, chest pain, and wheezing.
Too much exposure to bad ozone isn’t good for anyone, but it may actually make chronic respiratory diseases such as asthma and COPD worse.

How to Avoid Bad Ozone
The best way to avoid breathing ground level ozone is to live in a place where it doesn’t occur very often – someplace with lower population and industry, cooler temperatures, and lots of air movement (not in a valley).
If you can’t do that, keep an eye on the Air Quality Index (AQI) reports for your area, and plan accordingly.
Other things you can do:
-
-
- Stay indoors as much as possible when ozone/pollution levels are high.
- Keep windows closed.
- Use the circulate setting on your home thermostat to keep polluted air out.
- Exercise or be outside in the morning when ozone levels are lowest.
-
NOTE: Facemasks mandated for COVID-19 provide no protection against ozone.
If you do become exposed to bad ozone, just keep taking your prescribed asthma medications, but contact your doctor if problems persist.
Your lungs will usually recover within a few days after exposure to elevated concentrations of ozone.

Newest Treatments
Newer treatments, called Biologics, have been developed that make severe asthma easier to control.
Biologics
An estimated ~ 46,000 people with severe asthma may benefit from biologics, a new type of treatment some asthmatics call a “game-changer”.
Biologics are genetically engineered proteins that target the specific parts of the immune system that cause inflammation.
Clinical trials found that for those with severe asthma, using biologics can reduce asthma attacks by up to 50%. Your doctor may recommend treatment with biologics if you have severe asthma with symptoms not easily managed by other control medications.
If you start taking biologics, keep taking all of your other long-term or quick-relief asthma medications unless your doctor tells you to stop.
Biologic drugs work with your immune system to block the immune system chemicals that make your airways swell up.

Omalizumab
Omalizumab (Xolair) blocks the action of the immune system reaction that causes allergy and asthma symptoms.
Omalizumab is given by injection every 2-4 weeks. It isn’t generally recommended for children under 12.
In rare cases, this medication has triggered a life-threatening allergic reaction (anaphylaxis).
NOTE: Anyone who gets an injection of this drug should be monitored closely by health professionals in case of a severe reaction.
Eosinophils and Cytokines
A newer class of biologic drugs has been developed to target specific substances secreted by certain immune system cells.
These drugs target eosinophils and cytokines, reducing their numbers within the body and lowering inflammation.
These medications include:
-
-
-
- Mepolizumab (Nucala)
- Benralizumab (Fasenra)
- Reslizumab (Cinqair)
-
-
These drugs treat severe asthma that’s caused by a type of white blood cell called an eosinophil (eosinophilic asthma). You take them by injection or through an IV into a vein.
Tiotropium (Spiriva)
This inhaled medication has been used to treat chronic obstructive pulmonary disease (COPD) for more than a decade.
In 2015, the FDA also approved Spiriva for the treatment of asthma.
Studies show that tiotropium improves asthma control when added to high doses of inhaled corticosteroids plus short-acting beta-agonists.

Leukotriene Modifiers
One group of asthma drugs works by blocking the action of leukotriene – the chemical that narrows your airways during an allergic asthma attack.
Three leukotriene modifiers are approved to treat asthma:
-
-
-
- montelukast (Singulair)
- zafirlukast (Accolate)
- zileuton (Zyflo)
-
-
You take these medications by mouth to prevent or treat asthma attacks.
Bronchial Thermoplasty
Bronchial thermoplasty is a surgical technique used for severe asthma that hasn’t improved with other treatments.
During this technique, radiofrequency energy is applied to the airway.
The heat that’s generated destroys some of the smooth muscle lining the airway.
This treatment prevents the muscles of the airways from constricting and narrowing the opening.
Bronchial thermoplasty is delivered in three sessions, given three weeks apart.

Future Treatments
Researchers are still searching for new asthma drugs, and one that’s generated a lot of excitement is Fevipiprant (QAW039). If Fevipiprant is approved, it would be the first new oral asthma drug to be introduced in 20 years.
There’s no set date for Fevipiprant to be ready to use, but it’s in its final stages of study.

Other studies are identifying more specific triggers that set off asthma symptoms.
This could one day enable researchers to stop those processes and prevent asthma before it starts.
When making a decision about what meds to take, be sure to ask about any side-effects or interactions with other drugs you may be taking.
For instance, some drugs work by suppressing a natural response of the immune system, which could help your asthma, but it could also make you more vulnerable to infection.
So, be sure to weigh all of the pros and cons and talk it through with your doctor before starting any new treatment.

Progress in Treatment
Asthma as a disease has not changed for two centuries. But real progress has been made in identifying patients with asthma and its treatment.
-
- Doctors now know that allergic responses often substantially contribute to both chronic persistent asthma and acute asthma attacks.
- Recognition that asthma runs in families has also become the basis for very sophisticated studies of the genetics of asthma.
But in spite of all the progress, we still don’t understand the fundamental causes of asthma – there still is no cure.

How To Take Asthma Medications
Asthma Inhalers
Asthma inhalers are the most common and effective way to deliver asthma medicine to your lungs.
They’re available in several types that work in different ways. Your doctor might give you:
-
-
- A metered-dose inhaler, which uses a small aerosol canister to push out a short burst of medication through a plastic mouthpiece
- A dry powder inhaler, which releases the medicine only when you take a deep breath
-
I’ve used dry powder (crushed-pill) inhalers, which made me feel like I had pill-shrapnel stuck in my tonsils. I much prefer the aerosol (HFA) kind 🙂
Asthma Nebulizer
If you’re having trouble using small inhalers, your doctor may recommend a nebulizer.
A nebulizer converts liquid to a mist so the medicine is easier to get into your lungs. I call mine my “hookah” 🙂
I find the medicine administered from the nebulizer to provide more relief than from a regular hand-held inhaler.
It also has a mouthpiece or mask that makes it a good option for infants, small children, or anyone who has trouble using inhalers.
Treatments take about 20 minutes per dose. Nebulizers are portable, but must have access to an electrical outlet to run.

Keep Your Asthma Medicine Handy
Once you and your doctor have found a treatment or combination of medicines that work well for you, you’ll want to be sure to always have some handy.
You might also want to keep some extra, just in case 🙂
How to “Stockpile” Medications
Whether the supply chain has been disrupted by a natural disaster like a hurricane, Government lockdowns, or the spread of an infectious disease like COVID-19, people want to be prepared so they can stay as healthy as possible in the aftermath of an emergency.
It’s human nature to want to protect yourself and your loved ones.
These are some the common ways to stockpile extra medication:
-
-
-
-
- Refilling prescriptions early
- Paying for extra prescriptions
- Rationing medications
-
-
-
When considering these options, keep in mind that medications have expiration dates.
I store my medicine by expiration date, with the soonest to expire as the next inhaler to use.

Asthma Lifestyle Remedies
There are additional non-medical measures you can take – diet, exercise, supplements, or simply avoiding known triggers – that can also have a great impact on your asthma and overall health.
I personally prefer non-medical lifestyle solutions whenever I can use them, keeping daily medications and doctor visits to a minimum.
In addition to your medical treatment, you can try:
-
-
-
- Exercise
- Diet and Supplements
- Indoor air quality
-
-
For more ideas, just check out my Post Library for more asthma and Wellness related posts.
REFERENCES:

I hope this information about available prescription medical asthma treatments helps you improve your breathing and your overall health!
If you’re battling asthma and allergies, you might be interested in these other posts:
Asthma’s Effects on Mental Health
How Asthma and Allergies Change Over Time
Asthma and COVID-19: Are You at Higher Risk?
Clean Your Indoor Air With Houseplants!
Fight Asthma with Vitamins and Supplements
Eat to Breathe Easier – the Best Food for Asthma
Hiking With Asthma! A 3-Step Plan for Success
If you have a question, drop me an email and I’ll reply as soon as I can.
Thanks for stopping by – see you next time! LJ
To Get New Idratherwalk Posts
sent directly to your inbox (how convenient!) Click this Button
If you like this post, please share it!

LJ has spent much of her free time as a single Mom – and now as an empty-nester – hiking in the US and around the world. She shares lessons learned from adventures both local and in exotic locations, and tips on how to be active with asthma, plus travel, gear, and hike planning advice for parents hiking with kids and beginners of all ages. Read more on the About page.

